Original article (in Croatian) was published on 11/07/2023; Author: Ana Benačić
Health literacy is the ability of individuals to find, understand and use information and services, to make and take informed decisions and actions for the health of themselves and others.
The state of public health in Croatia is bad: Croatia ranks first in obesity, second in cancer mortality and fifth in smoking in the European Union. The number of new cancer cases in Croatia is approximately equal to the EU average, but Croats participate much less than the Union average in programs for the early detection of breast, cervical and colon cancer. Residents in rural areas and those with a lower level of education and income respond less often, according to the latest report of the Organization for Economic Cooperation and Development (OECD).
Poor concern about movement and nutrition, addictive behaviour and even missing preventive examinations in the world of health care are united under the name of health (il)literacy. The definition states that it is the ability of individuals to find, understand and use information and services, to make and take informed decisions and actions for the health of themselves and others. Costs arising from reduced health literacy in some countries are estimated to be three to five percent of the total cost of health care.
And the level of health literacy of Croatian citizens is, on average, on the very border between problematic and adequate. How many problems the citizens of the Republic of Croatia have with finding, understanding and using health information was examined for the first time in the research of Ana Bobinac, Elizabeta Ribaric and Nikolina Dukic Samarzija from the Faculty of Economics, University of Rijeka, presented in the scientific paper “Health Literacy in the Republic of Croatia” in the Social Review policy as part of the Health Observatory project. It is a consortium of associations and institutions to strengthen the influence of users, citizens, healthcare workers and healthcare researchers in political decision-making on health and healthcare.
Based on the research, the Guidelines for the Development of Public Policies authored by Maja Horvat were created, which should raise the level of health literacy. They were presented by the Krijesnica Association for Helping Children and Families Facing Malignant Diseases on July 10 in Zagreb.
Health consequences
Namely, people with a low level of health literacy take medicines incorrectly more often, go to the doctor more often, assess their own health as worse and use preventive protection measures less often, stay in the hospital more often and longer, use preventive examinations less often and generally increase the costs of the health system, while at the same time, it is more difficult for themselves and their loved ones to ensure a long and quality life.
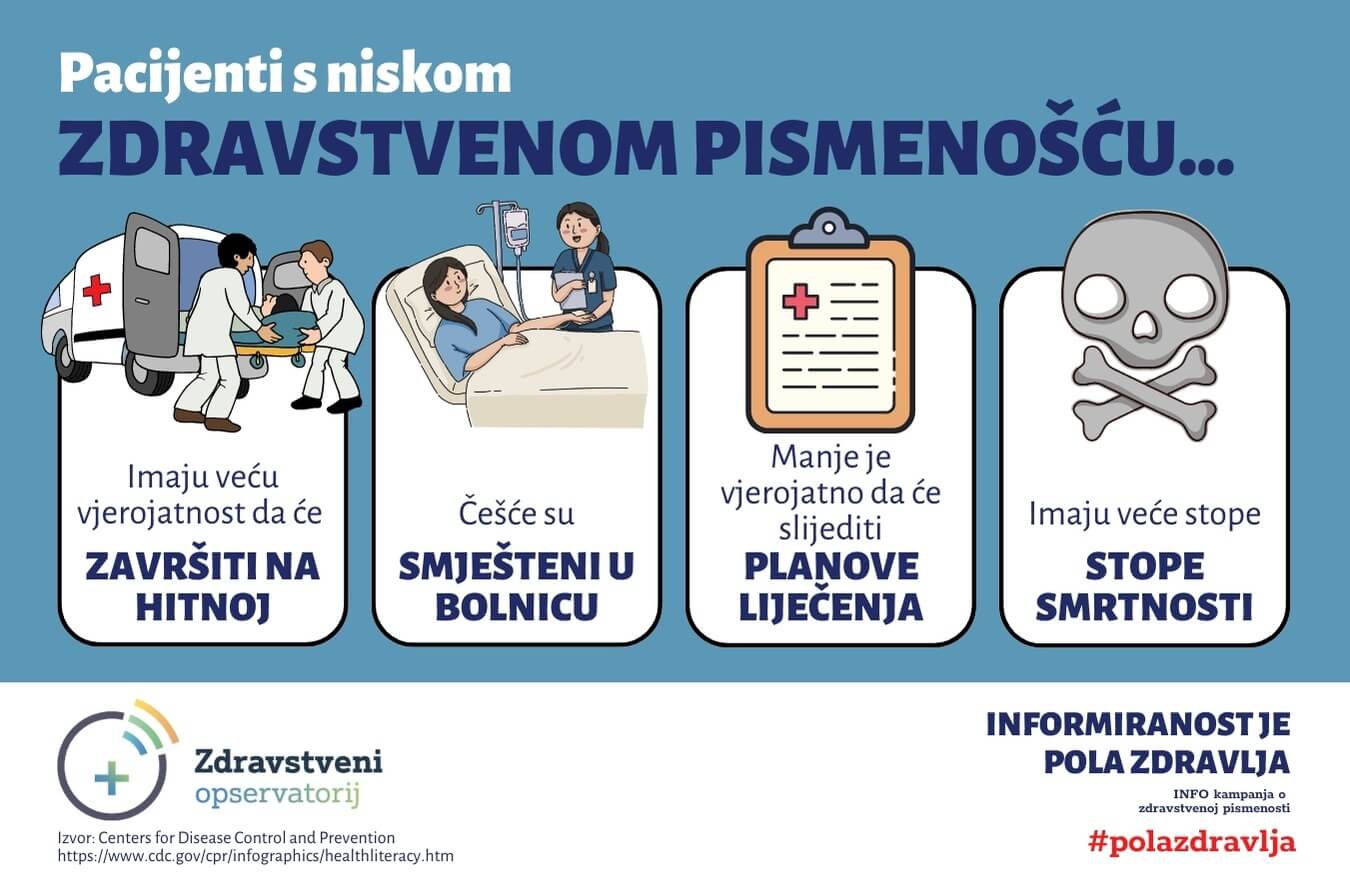
More often they rank themselves low on the social scale; have a higher body mass index – BMI; exercise less; have a lower income and find it difficult to make ends meet; have a lower level of education; they do not respond to preventive examinations and early cancer detection programs; they are older than 70 years.
One of the important determinants of health is good relations with doctors, as well as understanding their instructions. Noise in communication with doctors is often very expensive, but also dangerous. One US study, which reviewed medication error claims, estimated that between 2009 and 2013, the cost of poor communication was nearly two billion dollars, and nearly two thousand people died. The researchers stressed that this is probably the tip of the iceberg due to the cases that have not been prosecuted.
Confusing media
The main emphasis of the guidelines is that the lack of health literacy is not the sole responsibility of citizens and patients or even the media, which, according to respondents, have proven to be poor and incomprehensible informants about health.
More than 41 percent of the respondents do not know how to assess whether the information about health risks in the media is reliable; almost a third do not know how to read from the media how to protect themselves from illness, how to understand information on how to improve health or how to deal with problems related to mental health. There are many reasons for this – from the fight for clicks to short deadlines for publishing media articles.
However, Aleksandar Dzakula, a specialist in the organization of public health, considers the fact that the field of health expertise is fragmented to be a much bigger problem than the media, which fails to provide quality information.
“We have a lot of experts in hypertension, but there is no reference point, but a bunch of individual expertise”, Džakula pointed out. In a situation where there is no systematic authority for a certain area, patients get conflicting information from equally valuable professional sources and become victims of inadequate literacy, not health illiteracy. It is a disease of the Internet age; patients come armed with wrong information, because of which they are often frustrated and make unrealistic demands on healthcare professionals.
Educate healthcare workers
That is why the guidelines state that public campaigns should not rely exclusively on the media but on community work and the training of medical personnel. The obstacle to educating citizens to help themselves in Croatia is not only the fact that health education has been called into question by political struggles but also the fact that it is insufficient.
“You can’t focus on educating citizens and patients, but you need to educate the system and health personnel”, said Milan Kostro, presenting the guidelines.
According to the International Handbook of Health Literacy, there are several ways health professionals can help patients take adequate care of themselves.
One is feedback learning, a method of checking that the patient has understood the information provided. The person is asked to explain back what was said to him. The goal is to test the professional’s ability to explain the information, not the patient’s ability to understand it.
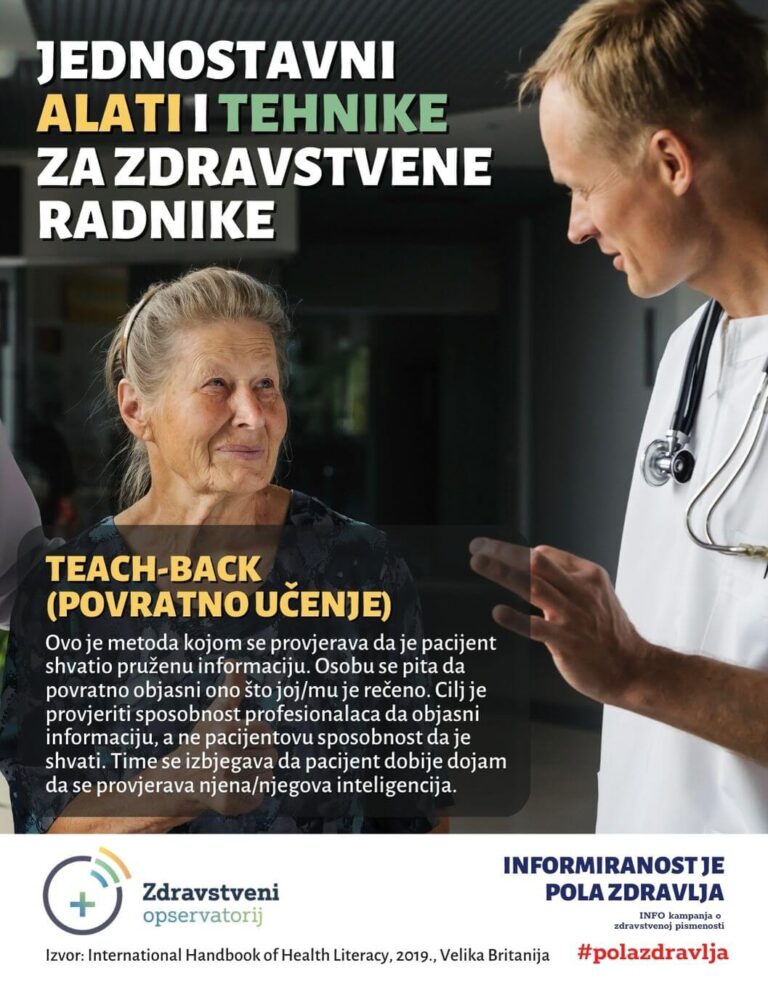
Furthermore, instead of providing more information at once, it is recommended to break the information into smaller and easier-to-understand units. Medical professionals are also encouraged to use plain language and images, as well as offer help with paperwork.
However, due to overload, doctors do not see themselves as people who will educate patients. Only one medical faculty in Croatia has communication as the subject.
That is why the proposed measures include improving the communication skills of doctors and other medical personnel towards patients; strengthening the role of pharmacists in the health literacy of citizens and the development of new and improvement of existing communication channels of public health institutions.
Other measures
The guidelines also suggest better labelling of medical spaces to make it easier for patients to find certain medical services, as well as improving the labelling of health-harmful products and services and developing new ways of informing about health. In addition to the media, it is necessary to strengthen the role and mandate of the Institute for Public Health and School Medicine concerning the development of health literacy programs, based on insight into regional and local conditions and needs.
It is also suggested to improve health literacy for vulnerable groups in the community, such as asylum seekers and Roma people.
The development of personal competencies of citizens for better finding, understanding, evaluating and using health information can be achieved by developing the critical thinking of young people and educating adults.
It is also recommended to encourage the development of the institutional framework, achieve better health literacy and monitor the effectiveness of future activities and record good practices, as well as repeat the measurement of the national level of health literacy.
Open drug discussions for patients
In addition to guidelines for health literacy, the observatory also made several recommendations, including those for drug policy. The public, that is, patients and their families, are completely excluded from the discussion on the inclusion of new drugs on the lists of the Croatian Institute for Health Insurance.
“Meetings of the Medicines Committee are not open to the public and there is no official mechanism for patients to contribute or receive any information about the process. The HZZO does not justify the inclusion of drugs on the lists at all, while the negatively evaluated proposals are argued with extremely short, templated explanations, from which it is not clear to the patients why a decision was made that the medicine is not financed from public funds”, the recommendations state.
Despite the significant increase in spending on medicines in the last ten years, which enabled great progress in the availability of new medicines to our patients, in 2021 only 35 of the 160 medicines registered with the European Medicines Agency from 2017 to 2020 were publicly financed in Croatia; many times less than in the more developed countries of Western Europe, but also significantly less than in most central European countries (Hungary, Czech Republic, Poland, etc.).
They point to Scotland as a positive example, which collects patient testimonials in the process of drug evaluation. The subject of formal statements prepared by patients includes the following: how the disease affects daily life, how well publicly funded drugs help patients manage their disease, whether the drug being evaluated would improve the patient’s quality of life, and how it would affect the patient’s family and those who provide them with care and whether the drug has any shortcomings compared to existing therapy.