Original article (in Serbian) was published on 29/09/2023; Author: Milica Ljubičić
According to data from 2020, Serbia ranks second in terms of deaths from cervical cancer in Europe, right behind Montenegro. Since last year, free vaccination of children up to 19 years of age with the HPV vaccine has started in our country, which largely prevents the occurrence of various types of cancer, including cervical cancer. Such horrifying statistics do not prevent anti-vaxxers from repeating again and again that the HPV vaccine is ineffective and that it affects fertility. There is no evidence that it reduces fertility, and numerous studies around the world show that the HPV vaccine is safe and effective, that is, that it significantly reduces the occurrence of cervical cancer.
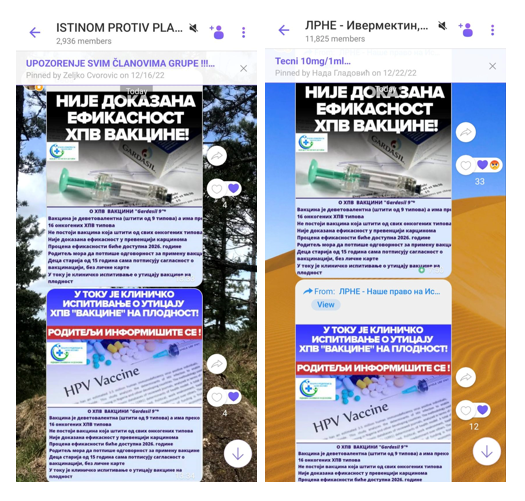
“The effectiveness of the HPV vaccine has not been proven”, states a post that we found in several groups on Viber. They share another post on the same topic: “A clinical trial is underway on the impact of the HPV vaccine on fertility”. Both posts show the logo of the citizens’ association “Doctors and Parents for Science and Ethics” which normally opposes the use of vaccines, claiming that they cause various diseases and disorders.
The Institute for Public Health “Batut” states that there are more than 120 types of human papillomavirus (HPV), of which about 40 can cause genital infections in men and women. These viruses can also lead to infection of the mucous membranes of the mouth and throat. Most infections caused by HPV pass without symptoms, that is, most infected people do not know they have an infection.
However, HPV infection can lead to various health problems, including the appearance of genital warts and various types of cancer in women and men.
This is precisely why the development of the HPV vaccine, which prevents infection with certain types of HPV, was a big deal in health history.
There are several vaccines for HPV infection, and the nine-valent Gardasil vaccine is given in Serbia, which was approved by the US Food and Drug Administration in 2014, and by the European Medicines Agency in 2015.
On the website of the American National Cancer Institute (NIH), it is stated that all vaccines that are in use so far, including Gardasil, have shown a high degree of effectiveness.
The American Medicines Agency (FDA) approved the quadrivalent Gardasil vaccine back in 2006, and it provided protection against infection with four types of HPV. The nine-valent version of this vaccine means an improved version because it protects against five more types of HPV.
It is estimated that this vaccine has the potential to prevent about 90 percent of cervical, vulva, vaginal and anal cancers.
The approval of this vaccine in the USA was preceded by a clinical study in which 14,000 women aged 16 to 26 participated and which showed that nine-valent Gardasil is even 97 percent effective in preventing cancer that can be initiated by an additional five types of HPV. In addition, this vaccine has proven to be effective in preventing diseases caused by four other types of HPV.
This vaccine has undergone several tests and is in use in other countries, including Great Britain and New Zealand, and is also used in Australia, which normally has a high level of vaccination against HPV.
Even a study published in The Lancet in 2018 predicts that if Australia maintains a high percentage of vaccination and screening, it will be the first country in the world to almost eliminate cervical cancer in the next 20 years.
On the website of our Institute for Public Health “Batut” it is stated that clinical trials “showed that the vaccine provides almost 100 percent protection against precancerous lesions and the quadrivalent HPV vaccine against genital warts caused by the types found in the vaccine”.
“Batut” points out that in the period from 2006, when the vaccine was first recommended, there was a 56 percent reduction in HPV infections among teenage girls in the USA, even though the HPV vaccination coverage was relatively low at that time. Research has also shown a reduction in the occurrence of genital warts in teenagers.
A study published in the medical journal The Lancet in November 2021 analyzed data since the introduction of the HPV vaccine for girls in England in 2008. The results show that the vaccine significantly reduced the number of precancerous growths and the occurrence of cervical cancer by 87 percent in women in their twenties who received the vaccine at the age of 12 or 13.
The scientists then estimated that by June 2019, 448 fewer cancers and about 17,300 fewer cancerous growths had been recorded over a period of 11 years.
And a study that was conducted in Sweden from 2006 to 2017 and included almost 1.7 million women and girls from 10 to 30 years of age, showed that the effectiveness of the HPV vaccine is especially pronounced in girls who were vaccinated before the age of 17.
HPV vaccines and fertility
In the disputed publication, it is also claimed that studies are underway on the impact of the HPV vaccine on fertility. However, it is not stated what kind of investigation it is, when it started, or who is conducting it.
Although it is possible that various research related to the HPV vaccine are being conducted, studies so far show that it is highly safe and does not affect fertility.
Anti-vaxers in Viber groups speculated earlier in the campaign against the HPV vaccine that it causes infertility, based on the claims of a motivational speaker who bragged on obscure channels that it had cured a mother of cancer, which we have already written about.
For example, a study from 2020, which was conducted in the USA, showed no evidence that there was an increase in infertility in women aged 18 to 33 who received the HPV vaccine.
“Batut” states that “there is no data suggesting that the use of the HPV vaccine could have effects on fertility”. They add that, however, there is a “possibility that the treatment of cervical cancer results in a woman’s inability to have a child”.
HPV infection is very common, i.e. one of the most common sexually transmitted infections.
“HPV infection is so common that almost all sexually active men and women are infected with some type of HPV at some point in their lives. Most people never find out that they have an infection, but they can pass it on to their partner without even realizing it”, writes “Batut’s website.
Since last year, all girls and boys between the ages of nine and 19 can receive the HPV vaccine in Serbia at the expense of the RFZO, before entering into sexual relations for the first time. According to the latest available data, about 27 thousand girls and boys have received it so far.
“Batut” states that even when someone has already had sexual relations, they can receive the HPV vaccine, but in that case, it provides partial protection, that is, it will protect against those HPV viruses to which the person was not exposed.
It is indicated that protection with the HPV vaccine is long-lasting and that, according to available studies, it lasts at least 10 years and does not lose its effectiveness. There is no data on whether the protection created after vaccination is lost over time.
According to data from the European HPV Center, cervical cancer is the fifth most common type of cancer that affects women in Serbia, and the second most common among women between the ages of 15 and 44. According to current estimates, every year 1,200 women are diagnosed with uterine cancer, and 600 die from the disease.
At the beginning of this year, “Batut” announced that based on the latest estimates of the European Information System for 2020, Serbia is still in the group with high rates of illness and death in Europe.
When it comes to cervical cancer, Serbia ranks fifth in Europe, after Montenegro, Romania, Estonia and Lithuania. In terms of deaths from cervical cancer, Serbia ranks second in Europe, after Montenegro.



